Please Walk Clockwise - Part 3
- 1 June 2020
This is part 3 in a series of three newsletters covering:
- Biomechanics of breathing
- Psychology of breathing
- Biochemistry of breathing
Part 1 - Biomechanics considered three key aspects:
- The importance of a good breathing rhythm, especially when running or walking to maintain social distancing.
- Droplet projection, especially if the exhale is bigger and more forced (e.g. with exercise).
- The significance of breathing through our nose vs mouth
Part 2 - The Psychology of Breathing considered three key aspects:
- Breathing has an influence on our neurochemical pathways, which has a flow on effect to how we feel, i.e. our moods, energy levels and emotions.
- The autonomic nervous system green zone and red zone
- The Vagus nerve
Part 3 considers:
- The main physiological roles of breathing
- When CO2 goes down- airway connection/muscle aches & fatigue
- The role of pH and homeostasis
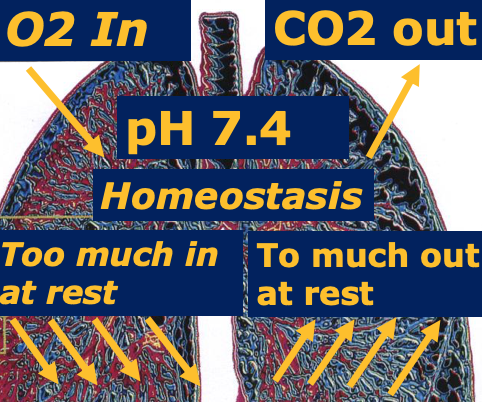
The key physiological functions of breathing are to breathe in oxygen and breathe out carbon dioxide whilst maintaining a stable body pH i.e. the acid-alkaline balance, this preserves homeostasis. Homeostasis is the stability/equilibrium within a cell and the body. If the pH alters for any reason our respiratory centre registers this change and will alter our breathing to keep everything stable. For example someone with unstable diabetes, lung disease or a pulmonary embolus will need to breathe faster or will present with an altered pattern to keep the body's pH stable. This breathing pattern is indicative something is not right. A qualified therapist is well versed and uses clinical reasoning skills to assess why someone has an altered breathing pattern and has the skills to treat appropriately.
It is important to seek a qualified breathing practitioner who is a medical professional such as a BradCliff Breathing Method practitioner.
Physiologically every cell in the body requires oxygen to survive and the body also needs to rid itself of carbon dioxide (CO2). CO2 is the most important stimulus for breathing in a healthy person.
When we over-breathe this means the way we breathe is not matching the activity e.g. breathing too fast, breathing upper chest and/or mouth-breathing. Mouth breathing at rest or during normal low-level activity can flush out too much carbon dioxide from the body.
When CO2 goes down
Although we all know how vital oxygen is, many people don't understand the importance of carbon dioxide. The carbon dioxide in our bodies regulates our breathing and our autonomic nervous system which controls all our organs.
Many things occur when blood levels of carbon dioxide are low, but here are a few key things that explain some scary symptoms especially related to airway health. This is highly relevant to anyone who has asthma, COPD or recovering from COVID 19.
Mast cells are rather like watchdogs lying in the tissues supporting the airways, give warning signals to the airways activating higher histamine levels in the blood and triggering broncho-constriction (tight pipes) and swelling of the linings of the airways. This is the lungs attempt to keep foreign invaders from entering the airways.
The airways tighten in response to lower blood CO2 levels, so do the arteries supplying other muscles, tissues and organs including the brain. In fact, blood flow to the brain may be reduced by as much as 50% during a bout of over-breathing. This often leads to feelings of suffocation and panic. Its hard to think clearly when this happens.Normal acid/alkaline balances (pH) in the body become altered. Over-breathing pushes CO2 levels to lower than normal, which tends to make the body tissues more alkaline. Tingling and light-headedness may be the first signs of this. But continued or chronic over-breathing becomes more complex as the body tries to adjust long-term to this state of affairs. The kidneys are called in to excrete bicarbonate (alkaline), helping retain normal body acid. The drive to breathe faster becomes habitual to maintain a normal pH (the body takes great pains to preserve this). CO2 levels remain lowered and the respiratory centre in the brain learns to accept this. The rest of the body is not quite so accepting. It suffers. This is the vicious cycle of habitual breathing dysfunction.
Low CO2 also stimulates lactic acid build-up in body cells as they attempt to balance their pH and metabolism is affected. Muscles ache, particularly the overused upper chest. These muscles are greedy for oxygen, stealing it away from lower back and leg muscles.
Over breathing / breathing dysfunction can can worsen asthma, induce breathlessness and panic plus add to muscle aches and fatigue.
All three functions described above are essential for health, energy, vitality and wellbeing.
This places breathing as the overseer of everything that happens in our body: in short, if breathing is not right it is difficult for any bodily function to work properly.
